Pregnancy is a unique life stage when women require special considerations, including increased attention to nutrition, physical activity, and food safety. This article will focus on key evidence-based dietary and nutrition recommendations specifically for pregnant women and their growing babies. A key resource for UGA Extension agents on this topic can also be found in chapter 5 of the Dietary Guidelines for Americans 2020–2025.
Nutrition plays a key role during pregnancy, for both the mom-to-be and her growing baby. While MyPlate and the Dietary Guidelines for Americans (DGAs) still apply during this stage of life, there are specific dietary recommendations that promote healthy pregnancy outcomes. These include prevention of chronic diseases for both women and babies, a decrease in pregnancy and birth complications, and healthy birth weights and outcomes.
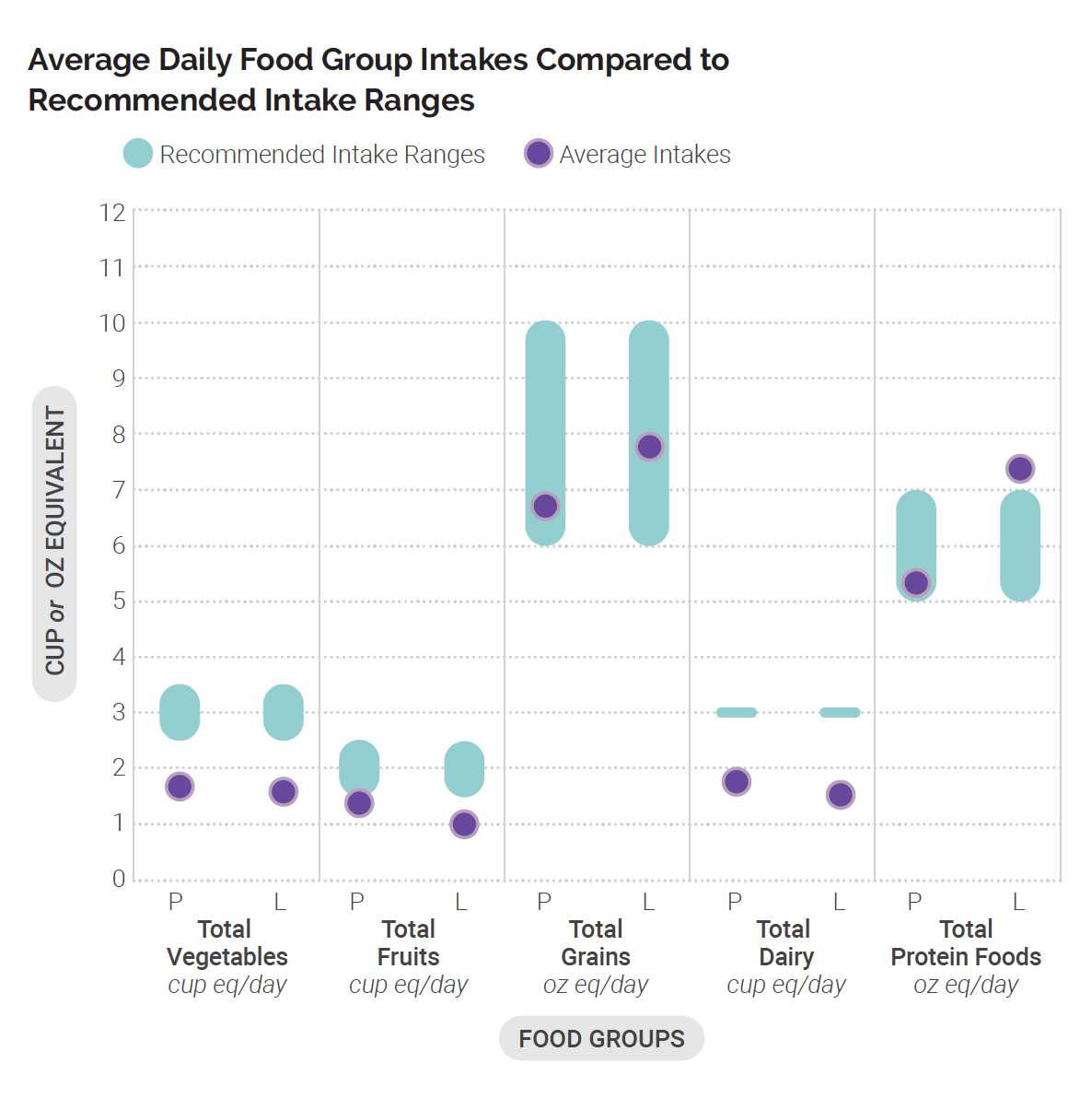
Pregnant women need nutrients from all five food groups: grains, fruits, vegetables, dairy, and protein foods. Recommendations for servings in each food group are similar to those for people who are not pregnant. For example, it is recommended that pregnant women consume 4–5 cups of fruits and vegetables each day; however, most pregnant women do not meet this guideline and often consume less than 2 cups of vegetables and 1 cup of fruit per day. It is also recommended for pregnant women to limit added sugars, saturated fat, and sodium.
Eating a variety of foods for an overall nutrient-dense diet is especially important during pregnancy. Variety ensures that pregnant women are able to meet their macronutrient needs (protein, carbohydrates, and fat) and micronutrient needs (vitamins and minerals). Pregnant women require an increase in specific nutrients during pregnancy, such as folate/folic acid, iron, iodine, and choline. Additionally, other special nutrition considerations include consumption of seafood, alcoholic beverages, caffeine, and prenatal supplements. The reality is that most pregnant women don’t meet these dietary and nutrient guidelines; therefore, it is important that they receive nutrition education in a variety of ways before and during pregnancy.
Nutrients for Special Consideration
Nutrients for special consideration are also important for pregnant women. These are nutrients that the general population should increase with their dietary intake, such as calcium, vitamin D, potassium, and dietary fiber. The calcium recommendation for 19- to 50-year-old adult women is 1,000 mg/day. For pregnant women who may already have a low calcium intake, the World Health Organization (WHO) recommends calcium supplementation up to 1,500–2,000 mg/day. The recommendation for Vitamin D (for 19–50-year-olds) is 600 international units (IU). There is some research to support that pregnant women may benefit from Vitamin D supplementation (taking 1000–4000 IU), but more research is needed to determine optimal amounts for promoting healthy pregnancy outcomes. See Table 1 for a summary of recommendations and food sources.
|
Nutrient |
Recommendation (women, 19–50 years old) |
Considerations during pregnancy |
Why it is needed during pregnancy |
Best food sources |
|---|---|---|---|---|
|
Calcium |
1,000 mg/day |
If calcium intake is low, supplementation of 1500–2000 mg/day can be beneficial |
Makes up bones and teeth |
Dairy: milk, yogurt; calcium-fortified orange juice, calcium-fortified soy milk |
|
Vitamin D |
600 IU/day |
Supplementation during pregnancy may be beneficial (1000–4000 IU/day) |
Promotes calcium absorption, maintains bone health |
Salmon, tuna, fish liver oils, egg (yolks), cheese, milk (mostly all milk in the U.S. is fortified with Vitamin D) |
|
Dietary Fiber |
At least 25 mg/day |
May help prevent constipation |
Promotes bowel health, may help decrease “bad” cholesterol in the blood |
Whole grains: brown rice, barley, whole wheat bread, pasta; fruits, vegetables, beans, peas, legumes, nuts, and seeds |
|
Potassium |
2,600 mg/day |
2,900 mg/day |
Essential mineral for proper functioning of heart, kidneys, fluid balance; contributes to lowering/controlling blood pressure, which is important for pregnant women and baby |
Excellent sources are fruits: apricots, prunes, raisins, bananas; vegetables: potatoes, squash; legumes: beans, peas, lentils; milk, yogurt, and chicken |
Nutrients for Special Consideration During Pregnancy
Dietary Guidelines for Americans 2020–2025 highlights several nutrients for special consideration for pregnant women. These nutrients are essential for a healthy pregnancy and the development of the baby.
Folate/Folic Acid

Folic acid is needed to prevent neural tube defects, which are birth defects of the spine, spinal cord, or brain. Spina bifida is an example and can occur within the first 28 days of pregnancy. A baby born with spina bifida will often have significant nerve and spinal cord damage. Since neural tube defects often develop during the first months of pregnancy, adequate folic acid is essential before pregnancy and during the first trimester.
Women who are planning to get pregnant should start taking a daily supplement of 400–800 µg of folic acid. This can be found in prenatal supplements, and it is also recommended that pregnant women take a prenatal supplement before and during pregnancy. The essential time period for folic acid supplementation is 1 month before pregnancy and through the first 3 months of pregnancy. Folate can be found in dark green vegetables, but additional folic acid is needed via supplementation in order to prevent neural tube defects.
Iron
Pregnant women have an increased need for iron because it is an essential nutrient that produces hemoglobin, which delivers oxygen from the lungs to the developing tissues of the baby. Iron deficiency, which can lead to anemia, is common in pregnant women, and almost one in four women develop iron deficiency in their third trimester. This can lead to complications during pregnancy, so it is important for women who are pregnant to take an iron supplement to meet the daily iron requirements of 27 mg/day. Iron can also be found in prenatal supplements.
Choline
Choline is an essential nutrient during pregnancy, as it is critical in the development of the baby’s brain, healthy growth and development of the spinal cord, and has an influence on cognitive function and the baby’s memory after they are born. Research also indicates that choline is important for maternal health during pregnancy for healthy liver function.
Choline deficiency has negative effects on the baby, including neural tube defects and impaired brain development, and it may also lead to maternal health complications such as hypertension and preeclampsia (high blood pressure in addition to potential damage to the kidneys and liver). It is important to note that choline is often not in prenatal supplements; separate supplementation may be needed to meet the increased requirements during pregnancy. Choline can be found in a varied dietary pattern of meats, fish, poultry, dairy, and eggs.
Seafood

While it may not be widely known, seafood consumption is strongly recommended during pregnancy. Research indicates that eating 8–12 oz of low-mercury seafood (e.g., salmon, tuna, clams) per week benefits the neurocognitive development of the baby and may improve IQ, communication, and other cognitive developments. Fish also provides essential nutrients such as omega-3 and omega-6 fats, iron, iodine, and choline. Seafood high in mercury, such as shark and swordfish, should be avoided during pregnancy, as methylmercury can be dangerous to the developing baby.
See Table 2 for a summary of these nutrients of special consideration during pregnancy, including food sources.
|
Nutrient |
Recommendation during pregnancy (women, 19–50 years old) |
Considerations during pregnancy |
Why it is needed during pregnancy |
Best food sources |
|---|---|---|---|---|
|
Folate/Folic Acid |
600–800 µg /day |
Supplementation is recommended starting at 1 month before pregnancy through the third trimester; found in prenatal supplements. |
Prevents neural tube defects |
Folate is found in dark green vegetables (spinach, asparagus), beans, peas, lentils, beef liver |
|
Iron |
27–30 mg/day |
Iron deficiency can lead to anemia and complications such as increased maternal/fetal mortality, premature birth, and low birth weight |
Needed for development of hemoglobin to carry oxygen from the lungs to body tissues; increased needs during pregnancy for the developing baby |
Heme iron best absorbed by the body: lean meat, seafood; Nonheme iron better absorbed with Vitamin C (and poultry/seafood): fortified cereals/grains, beans, peas, nuts |
|
Choline |
450 mg/day |
Consult with your doctor; supplementation is recommended before and during pregnancy; |
Promotes healthy development of brain and spinal cord, decreases risk of neural tube defects; may improve cognitive/memory function of baby |
Beef, egg, soybeans, chicken, fish, dairy; choline is found in smaller amounts in nuts, seeds, beans, whole grains |
|
Seafood |
8–12 oz per week |
Low-mercury fish is recommended; avoid high-mercury fish |
Neurocognitive development; also improves cognitive function of baby (after birth) |
Low mercury: salmon, tuna, clams, crab, shrimp; High mercury: avoid shark, swordfish, mackerel |
|
Caffeine |
Consult with doctor |
Consume less than 200 mg/day |
Caffeine is not needed or recommended; less than 200 mg/day appears safe to consume during pregnancy |
LIMIT TO: 8 oz coffee, 16–24 oz tea, or 48–52 oz caffeinated soft drinks |
|
Alcoholic beverages |
Do not consume any alcohol |
Any alcohol may have negative effects on development of the baby |
Alcohol is NOT needed or recommended at all during pregnancy |
Prenatal Supplements
When a woman is planning a pregnancy, this is the optimal time for her to talk with her doctor about prenatal care and recommendations. A prenatal supplement will also be recommended at this time, particularly because there is an increased need for folic acid and iron before and during the first stages of pregnancy. Prenatal supplements can be found over the counter, and women should look for those that contain calcium and vitamin D in addition to the recommended folic acid and iron. Even if a woman starts taking a prenatal supplement after she knows that she is pregnant, it is still important that she schedules regular appointments with her healthcare provider/OB-GYN for continued prenatal care.
There is a lot for pregnant women to think about for the health and safety of themselves and their babies. Starting with good nutrition and knowing their specific nutrition recommendations during this life stage sets baby and mom-to-be up for success and health. Stay tuned for the next topics in this series on maternal health, including food safety, physical activity, healthy weight gain during pregnancy, and more.
References
American College of Obstetricians and Gynecologists. (2023). Nutrition during pregnancy frequently asked questions. https://www.acog.org/womens-health/faqs/nutrition-during-pregnancy
Bramante, C. T., Spiller, P., & Landa, M. (2018). Fish consumption during pregnancy: an opportunity, not a risk. JEMA Pediatrics, 172(9). https://doi.org/10.1001/jamapediatrics.2018.1619
Centers for Disease Control and Prevention, Center for Nutrition Policy and Promotion, Food and Drug Administration, Food and Nutrition Service, FNS, SNAP-Ed Connection, & National Institutes of Health. (n.d.). Eye on nutrition: Potassium. U.S. Department of Agriculture WIC Works Resource System. https://wicworks.fns.usda.gov/resources/eye-nutrition-potassium#
Cleveland Clinic. (2025). Spina bifida. https://my.clevelandclinic.org/health/diseases/8719-spina-bifida
Committee on Obstetric Practice. (2010). Moderate caffeine consumption during pregnancy. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2010/08/moderate-caffeine-consumption-during-pregnancy
Institute of Medicine (US) Committee of Nutritional Status During Pregnancy and Lactation. (1990). Nutrition during pregnancy. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK235217/
Jaiswal, A., Dewani, D., Reddy, L. S., & Patel, A. (2023). Choline supplementation in pregnancy: current evidence and implications. Cureus, 15(11), e48538. https://doi.org/10.7759/cureus.48538
Mate, A., Reyes-Goya, C., Santana-Garrido, Á., & Vázquez, C. M. (2020). Lifestyle, maternal nutrition and healthy pregnancy. Current Vascular Pharmacology, 19(2), 132–140. https://doi.org/10.2174/1570161118666200401112955
Mayo Clinic Staff. (2024, December 11). Dietary fiber: Essential for a healthy diet. Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983
Mayo Clinic Staff. (2025a, January 31). Iron deficiency anemia during pregnancy: Prevention tips. Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/anemia-during-pregnancy/art-20114455
Mayo Clinic Staff. (2025b, March 1). Prenatal vitamins: Why they matter, how to choose. Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-vitamins/art-20046945
Office of Dietary Supplements. (2022a, June 2). Choline fact sheet for health professionals. National Institutes of Health. https://ods.od.nih.gov/factsheets/Choline-HealthProfessional/
Office of Dietary Supplements. (2022b, June 2). Potassium fact sheet for health professionals. National Institutes of Health. https://ods.od.nih.gov/factsheets/Potassium-HealthProfessional/
Office of Dietary Supplements. (2022c, November 30). Folate fact sheet for health professionals. National Institutes of Health. https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
Office of Dietary Supplements. (2025a, June 27). Vitamin D fact sheet for health care professionals. National Institutes of Health. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
Office of Dietary Supplements. (2025b, July 11). Calcium fact sheet for health professionals. National Institutes of Health. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
Pari-Keener, M., Gallo, S., Stahnke, B., McDermid, J. M., Al-Nimr, R. I., Moreschi, J. M., Hakeem, R., Handu, D., & Cheng, F. W. (2020). Maternal and infant health outcomes associated with medical nutrition therapy by registered dietitian nutritionists in pregnant women with malnutrition: an evidence analysis center systematic review. Journal of the Academy of Nutrition of Dietetics, 120(10), 2730–1744. https://doi.org/10.1016/j.jand.2019.10.024
Pérez-López, F. R., Pilz, S., & Chedraui, P. (2020). Vitamin D supplementation during pregnancy: an overview. Current Opinion in Obstetrics and Gynecology, 32(5), 316–321. https://doi.org/10.1097/GCO.0000000000000641
U.S. Department of Agriculture, & U.S. Department of Health and Human Services. (2020). Dietary Guidelines for Americans 2020–2025. https://www.dietaryguidelines.gov/sites/default/files/2021-03/Dietary_Guidelines_for_Americans-2020-2025.pdf
U.S. Food and Drug Administration. (2022). Questions & answers from the FDA/EPA advice about eating fish for those who might become or are pregnant or breastfeeding and children ages 1 to 11 years. https://www.fda.gov/food/consumers/questions-answers-fdaepa-advice-about-eating-fish-those-who-might-become-or-are-pregnant-or
World Health Organization. (2023). E-Library of evidence for nutrition actions (eLENA). https://www.who.int/tools/elena/interventions/calcium-pregnancy