Diabetes is a chronic disease that affects how your body processes blood glucose (sugar). Managing diabetes effectively is essential to maintaining overall health. One of the most critical aspects of diabetes management is routine blood glucose monitoring. This practice helps people with diabetes make informed decisions about their diet, physical activity, and medication, ultimately reducing the risk of serious long-term complications (American Diabetes Association [ADA], n.d.-a, n.d.-d).
Risks of Not Monitoring Your Blood Glucose
According to the ADA, poorly managed diabetes can lead to severe health problems such as cardiovascular disease, nerve damage (including neuropathy and gastroparesis), foot and skin problems, and diabetic ketoacidosis.
Neuropathy is nerve damage, which can cause pain, numbness, or loss of sensation, particularly in the feet, making injuries harder to detect and impairing wound healing. These issues, combined with poor blood circulation, can lead to ulcers or amputation.
Diabetic ketoacidosis (DKA) is a life-threatening condition where the body, lacking insulin, breaks down fat too quickly, producing acids called ketones. The buildup of ketones in the blood causes blood to become acidic (ketoacidosis), which can lead to coma or death without rapid medical intervention (ADA, n.d.-a).
Fortunately, accurate blood glucose self-monitoring can help prevent or delay these complications. To help ensure accurate blood glucose monitoring, follow these steps carefully.
Why Blood Glucose Monitoring is Important
Blood glucose monitoring is essential for managing type 1 and type 2 diabetes. It is the most effective way to check whether your blood glucose levels are within the range recommended by your healthcare provider. By monitoring your blood glucose levels on a regular basis, you gain valuable insights into how your diet, physical activity, and medications affect your blood glucose, which empowers you to make informed decisions to effectively manage your diabetes.
Monitoring also helps you recognize patterns and allows you to take timely action to prevent highs and lows. It eases uncertainty and provides peace of mind, reassuring you that you are managing your condition effectively and staying on track with your health goals (Centers for Disease Control and Prevention, 2024).
When to Check Your Blood Glucose
The frequency of testing should be tailored to your individual treatment plan. However, common times to check include:
- before meals or snacks
- when you feel symptoms of high or low blood sugar
- before driving (to ensure safe glucose levels)
- before and after exercise
Your healthcare provider may also recommend testing:
- when fasting
- before going to sleep
- upon waking up (ADA, n.d.-c)
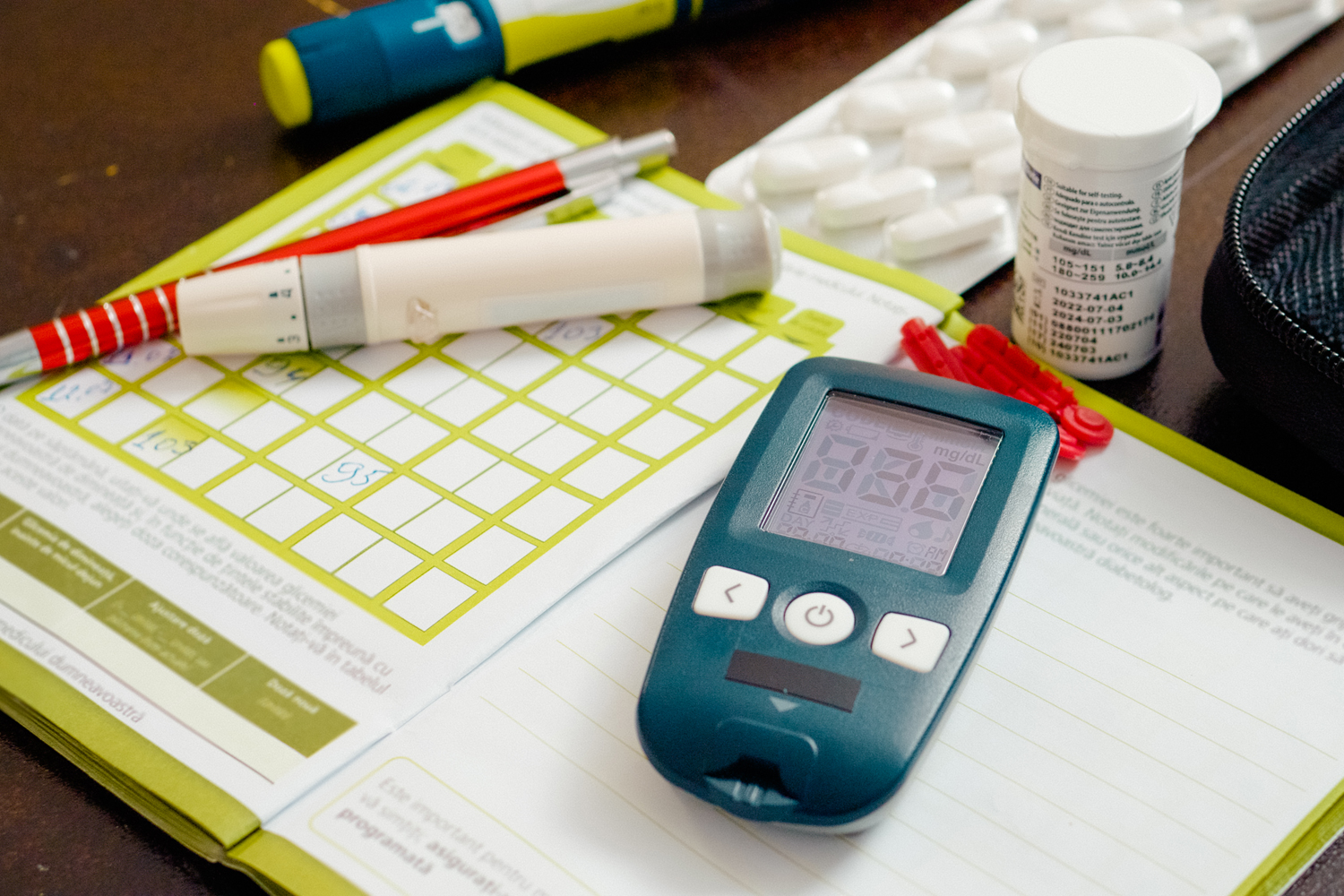
Blood Glucose Meters
Blood glucose meters (BGMs), also called glucometers, are one of the most commonly used tools to check blood glucose levels. BGMs are portable, digital devices that provide accurate and timely information to help individuals manage their diabetes effectively. Most BGMs measure glucose in whole blood. The meter displays a blood glucose level on a digital screen within seconds.
BGMs work by analyzing a small drop of blood, usually obtained from the finger, applied to a blood glucose test strip. The ADA recommends using the side of the fingertip as the primary testing site and rotating fingers to avoid soreness in any one area.
Steps for Monitoring Blood Glucose Using a BGM
- Gather your supplies: a blood glucose meter, a lancet device (used to prick the skin), test strips, and a method for tracking your results. Many people, especially those who prefer traditional methods such as a blood glucose record book or blood glucose log over technology, will use these logs to identify patterns in their blood glucose levels.
- Check the expiration dates on the test strips. Expired strips can lead to inaccurate readings.
- Wash your hands thoroughly to remove any food or other residue that could affect the result. If soap and water are not available, you may use an alcohol prep pad to clean the fingertip—just be sure to let the area air‑dry completely before testing to avoid diluting the sample or interfering with the glucose reading.
- Insert a test strip into the meter.
- Load a new lancet into the lancet device and gently prick the side of your fingertip.
- Place a small amount of blood on the test strip in your meter. It only takes a few seconds for your result to appear on the screen.
- Record your result (ADA, n.d.-c; Mayo Clinic, 2023).
Additional Tips
- Use the side of your fingertip to reduce discomfort.
- Avoid over-squeezing your finger, which can impair the accuracy of the reading.
- Warming your hands may make it easier to get enough blood on the strip for testing. To warm your hands, wash them with warm water or gently rub them together before testing.
- Ensure your meter has sufficient battery life before testing.
Continuous Glucose Monitors
Continuous glucose monitors (CGMs) are devices that provide real-time updates on your blood glucose levels through a small sensor worn on the body. According to the ADA, CGMs are becoming increasingly popular among individuals with type 1 and type 2 diabetes, and they are known for their high accuracy. CGMs are usually recommended for people using insulin treatments, such as insulin pumps or injections.
To use CGM, a small sensor is inserted under the skin, typically on the abdomen or upper arm. This sensor continuously measures glucose levels in the body’s interstitial fluid and transmits the data to a display device, which may be a smartphone app, a receiver, or an insulin pump.
The most commonly used CGMs are:
- Dexcom G6 and G7
- Medtronic Guardian 3 or 4
- Abbott Freestyle Libre 2 and 3
Each of these systems offers reliable glucose tracking. Your endocrinologist or primary care provider can help you determine which is most effective for your needs.
Benefits of CGMs
Compared to traditional BGMs, CGMs offer several advantages, such as:
- providing warning notifications when blood glucose is too low or too high,
- eliminating the need for finger sticks,
- allowing for data sharing with your healthcare provider,
- reducing the risk of hypoglycemia (low blood glucose levels) and hyperglycemia (high blood glucose levels), and
- allowing for better trend tracking and more informed treatment decisions (ADA, n.d.-b).
Hemoglobin A1C Test
A hemoglobin A1C test, or HbA1c, is a laboratory test ordered by your healthcare provider. It measures your average blood glucose levels over the past 2 to 3 months, offering a broader view of your long-term glucose control.
An A1C test helps determine how close your blood glucose levels are to your target range over time. While A1C test kits can be purchased over-the-counter (without a prescription), these “at-home” tests are not as accurate as laboratory tests that are completed at your doctor’s office (Jacobsen et al., 2022). Your doctor will provide your A1C result and set a personalized goal, which typically ranges between 5.7% to 10% depending on your health status and treatment plan.
Summary
Monitoring your blood glucose, whether through BGMs, CGMs, or A1C testing, is a vital part of diabetes management. Consult with your healthcare provider to determine which tools and strategies are best suited to your lifestyle and treatment goals (ADA, n.d.-e).
References
American Diabetes Association. (n.d.-a). About diabetes: Diabetes complications. Retrieved July 11, 2025, from https://diabetes.org/about-diabetes/complications
American Diabetes Association. (n.d.-b). About diabetes. Choosing a CGM. Retrieved August 19, 2025, from https://diabetes.org/about-diabetes/devices-technology/choosing-cgm
American Diabetes Association. (n.d.-c). Cracking the Code: Using a Blood Glucose Meter. Retrieved January 11, 2025, from https://professional.diabetes.org/sites/dpro/files/2023-12/usingabloodglucosemeter.pdf
American Diabetes Association. (n.d.-d). Treatment & care. Check your blood glucose | Diabetes testing & monitoring. Retrieved August 19, 2025, from https://diabetes.org/living-with-diabetes/treatment-care/checking-your-blood-sugar
American Diabetes Association. (n.d.-e). Understanding A1C: What is the A1C test? Retrieved July 11, 2025, from https://diabetes.org/about-diabetes/a1c
Centers for Disease Control and Prevention. (2024, May 15). Monitoring your blood sugar. Retrieved July 11, 2025, from https://www.cdc.gov/diabetes/diabetes-testing/monitoring-blood-sugar.html
Cleveland Clinic. (2024, January 17). Insulin. Retrieved July 1, 2025, from https://my.clevelandclinic.org/health/body/22601-insulin
Jacobsen, L. M., Bocchino, L. E., Lum, J. W., Kollman, C., Barnes-Lomen, V., Sulik, M., Haller, M. J., Bode, B., Cernich, J. T., Killeen, A. A., Garg, U., Liljenquist, D., Adams, J. G., Clements, M., Gabrielson, D., Johnson, T., Clements, M. A., & Beck, R. W. (2022). Accuracy of three commercial home-use hemoglobin A1c tests. Diabetes Technology & Therapeutics, 24(11), 789–796. https://doi.org/10.1089/dia.2022.0187
Mayo Clinic. (2023, 15 Dec). Blood glucose monitors: What factors affect accuracy? Retrieved August 8, 2025, from https://www.mayoclinic.org/diseases-conditions/diabetes/expert-answers/blood-glucose-monitors/faq-20057902